Type 1 diabetes can develop at any age, is often confused with Type 2, and requires insulin to survive. Early signs can be subtle—here’s what to watch for, how testing works, and how parents can support their child’s care.
At a Glance:
- Autoantibody testing confirms diagnosis
- Autoimmune: attacks insulin-producing cells
- Can appear at any age
- Requires lifelong insulin
- Early signs: weight loss, thirst, frequent urination
As a mom of a child with an autoimmune disease (plus a health columnist and daughter of a nurse and a surgeon), I thought I was perceptive and observant enough to be able to catch medical issues early until my son lost a lot of weight in a matter of weeks. I first noticed he was looking a little thinner, but thought nothing of it, and since he wears baggy clothes, it wasn’t as apparent … until one day when I caught a glimpse of his collarbone protruding so much I could see the whole bony outline.
I asked him to weigh himself, if only to placate me. One step on the scale was enough to see the doctor. He had lost 20 pounds. Something was wrong.
At his primary doctor’s, his blood glucose was sky high at nearly 300, and a week later, he would be hospitalized, headed straight toward diabetic ketoacidosis. He tested positive for 3 out of the 4 antibodies for Type 1 autoimmune diabetes and was started on insulin immediately in the hospital. We were told he would have to take insulin several times a day for the rest of his life.
Psst… Check Out Where to Find the Best Pediatric Emergency Care in NYC and Beyond
How Did This Happen?
He was a healthy eater, active, and had regular check-ups. Of course, I started reading everything I could on the subject, joined parent groups, and listened to our endocrinologist and diabetic educator.
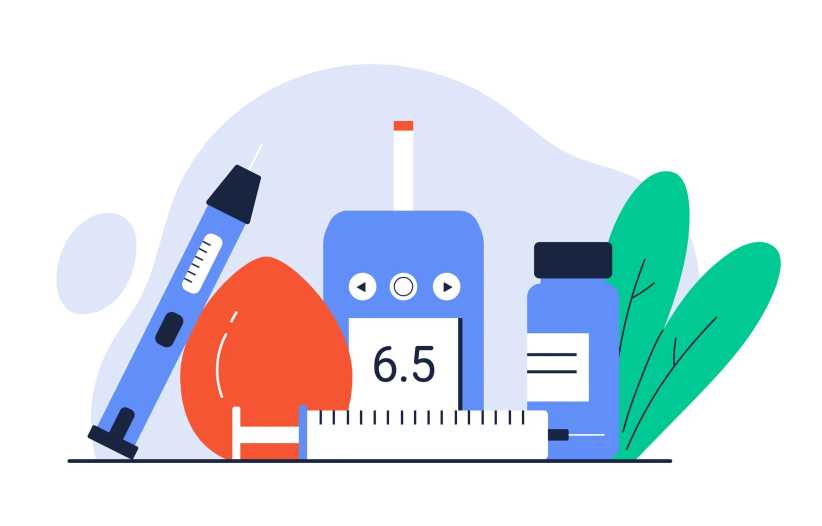
Since then, it’s been a whirlwind of learning about blood sugars, carb ratios, continuous glucose monitors (CGMs), insulin dosing, short-acting insulin (bolus), long-acting insulin (basal), all the various brands of each, pumps, sensors… the list goes on and on. Any parent of a Type 1 diabetic knows that the learning curve is steep and never really ends.
What Is Type 1 Diabetes?
Type 1 diabetes is an autoimmune condition in which the body attacks the insulin-producing cells in the pancreas. As a result, the body stops making insulin, a hormone needed to move glucose from the bloodstream into cells for energy.
“In diabetes, there’s a disruption in the immune system for reasons we’re not totally clear about,” explains Christopher J. Romero, MD, a pediatric endocrinologist at Mount Sinai Kravis Children’s Hospital, and Associate Professor of Pediatrics at Icahn School of Medicine at Mount Sinai. “It starts to react against the cells that make insulin, called beta cells. Eventually, those cells start to die, and then you’re not making insulin.”
Insulin is essential for survival because it allows glucose to enter the body’s cells for energy; without it, blood sugar rises to dangerous levels, and the body begins breaking down fat in a way that can quickly become life-threatening.
For a child (or adult) with Type 1 diabetes, giving them insulin is what keeps them alive. People with Type 1 diabetes need insulin for life. It’s a non-negotiable and not something that can be replaced with diet or exercise.
Without insulin, glucose cannot enter the cells to provide energy, and the body begins to shut down. Administering insulin, whether by injection or pump, allows the body to function, organs to work properly, and blood sugar levels to stay within a safe range.
Signs of Type 1 Diabetes That Can Often Be Missed
Type 1 diabetes can come on fast, and early symptoms are easy to overlook in active kids. Dr. Romero points out, “In type 1 diabetes, technically by the time you see symptoms, that beta cell mass is already decreased by 75-80%, so most of your cells are gone.”
Signs and symptoms:
- Extreme thirst
- Frequent urination (including new bedwetting)
- Sudden weight loss
- Fatigue or irritability
- Blurry vision
Not everyone experiences all of these symptoms, and when they do appear, they’re often subtle.
Misdiagnosis Is More Common Than You May Think
Because Type 1 diabetes is still widely misunderstood, it’s sometimes missed or misdiagnosed, especially in older kids, teens, and adults. Some clinicians were trained back when Type 1 was considered a childhood disease and Type 2 an adult one, so new-onset Type 1 can be mistaken for Type 2 or not fully evaluated.
If symptoms are present, it’s important to push for blood sugar testing and diabetes autoantibody tests. These simple blood tests look for markers like GAD, IA-2, and ZnT8 antibodies that show the immune system is attacking insulin-producing cells. When those antibodies are present, it confirms Type 1 diabetes and signals the immediate need for insulin.
Early testing can prevent Diabetic Ketoacidosis (DKA), a life-threatening complication. DKA occurs when the body doesn’t have enough insulin to allow blood sugar into the cells for use as energy. Instead, your liver begins to break down fat for fuel, a process that produces acids called ketones. When too many ketones build up too quickly, they can poison the body, leading to a coma or death if not treated immediately in a hospital.

After Type 1 Diagnosis
Administering Insulin
Giving insulin can be frightening, whether you’re doing it for your child or trusting your teen to manage it themselves, especially knowing that insulin can cause dangerous lows. That’s why diabetes education is vital. Even with training from your child’s doctors and nurses, parenting a child with Type 1 diabetes requires ongoing vigilance: checking blood sugars, watching trends, and responding fast when numbers shift.
Unlike other diseases that can be treated with a standard medication dosage, insulin needs change throughout the day, depending on food, activity, sleep, sickness, and other factors.
Part of the problem is that every human body responds differently to how blood sugar and insulin are used, and it takes a lot of trial and error to figure out your child’s insulin needs. Then, when you do, it’s common for that to change due to hormones, growth, stress, and other factors.
Honeymoon Period
There is also what doctors refer to as a honeymoon period in Type 1 diabetes, where a person still has some insulin, which may make figuring out insulin units tricky. This period can be somewhat cruel because it can give parents a false sense of “maybe they’re getting better” before the pancreas fully stops. Eventually, insulin needs will increase as the body’s natural insulin depletes entirely.
Informed experimentation is a hallmark of treating Type 1 diabetes, because insulin needs can shift day to day, and what worked yesterday may suddenly be too much or not enough today, as every body responds differently to constantly changing variables.
It Takes Time
“The impulse of any parent is ‘ok, I need to fix this right now’ but there is some guessing to it, it’s educated guessing but it’s guessing, and can be very challenging, says Dr. Romero.
With new patients, he breaks it down to simple concepts, instructs parents on the basics first, such as what a low blood sugar is, what a high blood sugar is, and the mechanics of how to treat each of them.
Dr. Romero tells his patients, “We are going to work to make these blood sugars better, but the first thing you need to do is take care of your child and help them transition to this new condition. If you can do that, along the way, we start to individualize the care for the child. It’s an ongoing education.”
If this seems overwhelming, it is, and exhaustion is a side effect. CGM alarms can go off at all hours, pulling you and your child out of sleep. Some nights it means giving insulin; others it means waking your child to eat or drink to treat a low, something that can turn serious quickly if missed.
School and Type 1 Diabetes
At school, children need immediate access to insulin and fast-acting sugar at all times, in every classroom, on the playground, and on field trips.
In New York City, students with Type 1 diabetes are protected under federal law and entitled to accommodations like 504 Plans and trained staff. But those protections only work when the staff understands the seriousness of the disease: a child should never be sent alone to the nurse, delayed in treatment, or denied insulin or glucose when they need it.
Many parents say that connecting with other families who understand, often online, in the middle of the night, is what makes them feel less alone. I can attest to that. I have spent many nights asking questions and finding comfort in the advice of those who have navigated the same ups and downs- and still do. You don’t have to navigate this journey alone. If your family is managing a Type 1 diagnosis and you would like to connect or ask questions, please feel free to reach out via email.

Type 1 Diabetes Resources for NYC Families
Medical Resources
- Breakthrough T1D (Formerly Juvenile Diabetes Research Foundation- JDRF)
- American Diabetes Association
- Children with Diabetes
- Beyond Type 1
- NYC Pediatric Endo Programs: Look into specialized care at Mount Sinai, NYU Langone, or NewYork-Presbyterian
- Diabetes camps
Online Parent & Community Support
- Facebook groups for parents of kids with Type 1 diabetes (including age-specific and newly diagnosed groups)
- Instagram and Threads T1D advocacy communities
- Reddit communities such as r/Type1Diabetes and r/diabetes_t1
Psst… Check Out Barbie Debuts First-Ever Barbie Doll with Type 1 Diabetes