Your winter survival guide: Help your baby fight off the flu and other cold-weather bugs with our expert advice on how to handle a variety of seasonal symptoms.
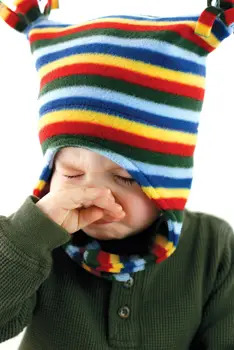 Even if this is your baby’s first winter, you’re probably prepared for a few cases of the sniffles. It’s those other winter bugs – the ones that can cause soaring fevers or awful coughs – that leave you rattled. But not for long: We walk you through the latest research on seasonal bugs that strike babies and provide expert tips on the best ways to fight back.
Even if this is your baby’s first winter, you’re probably prepared for a few cases of the sniffles. It’s those other winter bugs – the ones that can cause soaring fevers or awful coughs – that leave you rattled. But not for long: We walk you through the latest research on seasonal bugs that strike babies and provide expert tips on the best ways to fight back.
“How can I tell the difference between a cold and the flu?”
Fatigue, fever, cough, and runny nose are classic signs of the flu, but some infants’ only symptoms may be irritability, difficulty sleeping, and rapid breathing, says Robert Baltimore, M.D., professor of pediatrics and epidemiology at Yale University in New Haven, Connecticut. A characteristic of the H1N1 flu is vomiting and diarrhea. A simple cold will generally not prompt fevers, phlegmy coughs, or severe irritability.
Babies are among the most vulnerable to complications from flu viruses, including dehydration (watch for fewer wet diapers and/or dark urine), ear infections, and bacterial pneumonia, which is often characterized by a high fever, severe coughing, and trouble breathing. This is why seasonal and H1N1 flu vaccines are so strongly recommended for babies six months and older. If your infant is younger than that, everyone in your family – and anyone who has regular close contact – should be immunized for both the seasonal flu and the H1N1 flu, says Jennifer Shu, M.D., coauthor of Heading Home With Your Newborn (American Academy of Pediatrics). The flu season often doesn’t peak until March, so your child could still benefit from getting the vaccine now.
Best Treatments for the Flu: The virus often takes a week or more to run its course, so all you can do is ease her symptoms. Offer formula or the breast more frequently to prevent dehydration; consider elevating the mattress in her crib; and use saline nose drops and/or a humidifier to relieve stuffiness. You can also try a nasal aspirator to suction out mucus. Ask your doctor about giving a pain/fever reducer to help keep her comfortable.
“What if the cough is persistent and severe?”
Pertussis (also known as whooping cough) is a highly contagious bacterial infection that is tricky to catch early because it starts out like a cold, with sneezing, runny nose, and a mild cough, which usually worsens after the first few days of infection. Then after one or two weeks, often after the cold symptoms appear to subside, severe coughing spells begin. Babies will cough repeatedly (sometimes 10 to 15 times in a row), then take in a high-pitched breath (the whooping sound). Vomiting may follow. Prepare yourself: The cough can last as long as six weeks. Babies younger than six months are especially vulnerable because they’re too young to be fully vaccinated. Up to 75 percent of infants younger than six months old who contract the disease must be hospitalized.
Best Treatments for Whooping Cough: The CDC recommends that all adults receive the pertussis booster Tdap if it’s been 10 years since their last shot (and sometimes sooner). This is because about 90 percent of susceptible people in a home contract whooping cough after exposure, and babies can catch the illness from parents or siblings whose immunity has waned. The shot is recommended for babies at two, four, and six months, with boosters at 15 to 18 months and 4 to 6 years. If your baby develops cold symptoms after coming in contact with someone with whooping cough, your doctor may start antibiotics immediately, which can shorten the course, the severity, and the spread.
For an infant diagnosed with the full-blown illness, expect a course of antibiotics to prevent further transmission. Though it’s difficult to watch your baby coughing relentlessly, the most important thing you can do is to try to keep him calm – read to him, play soothing music, give lots of hugs – whatever works. You can also use a cool-mist vaporizer to help loosen respiratory secretions and soothe irritated lungs and breathing passages. (Be sure to follow directions for keeping the vaporizer clean and mold-free.) In addition, keep your home free of irritants that can trigger coughing spells, such as aerosol sprays, tobacco smoke, and smoke from cooking, fireplaces, and wood-burning stoves. Children with whooping cough may vomit or not eat or drink much because of frequent coughing. Offer smaller, more frequent meals and encourage your child to drink lots of fluids.
“My little cutie sounds like a barking seal.”
If your bambino comes down with cold symptoms and a fever and then becomes hoarse, she may have contracted croup, a virus that settles into the voice box and causes swelling in this narrow part of the airway. The hoarseness may result in an often scary-sounding barking cough. Some children also may make a high-pitched whistling noise called stridor while inhaling, a condition that requires immediate evaluation. Symptoms tend to be more severe at night, says Baltimore.
Although croup is one of those coughs that can sound more dangerous than it actually is (most cases are mild), babies younger than 18 months are at higher risk for complications because their airways are so small to begin with, says Baltimore.
If you notice pulling below your baby’s ribs when she inhales, that she’s leaning forward to breathe, and/or that she’s panting, wheezing, or turning blue, don’t wait – call 911.
Best Treatments for Croup: Despite a lack of hard evidence, doctors have long advised sitting with the baby in the bathroom for 10 minutes while running a steamy shower. You can also try taking your child outside (if it’s not too cold) for a few minutes to breathe in the cool air – both techniques appear to help reduce inflammation. Babies with more severe cases (the coughing is interfering with eating, drinking, and sleeping) may benefit from a short course of steroid treatment. The medicine can buy your child 24 hours of relief, getting her through the worst of what’s usually only two days of symptoms, says Baltimore.
“My baby seems to have a stomach bug in addition to cold symptoms.”
When fever is accompanied by vomiting and watery diarrhea that may be quite green (the symptoms often occurring in this order) it may be rotavirus, says Baltimore. Abdominal pain is also common. You’ll know your little one may have a tummy ache if he draws his legs up to his belly, seems uncomfortable when you press on his stomach, and refuses to eat.
The risk of dehydration is one of the biggest worries for babies who get nabbed by this highly contagious bug, which spreads through contaminated fecal matter. About one in 40 will need to be hospitalized for intravenous fluids and other care, according to the CDC.
Best Treatments for Rotavirus: You now have the option of vaccinating your child against rotavirus, but your baby needs to receive the series of three shots before he’s 32 weeks old. If your little one missed the window and becomes infected, your main goal is to keep him hydrated, hydrated, hydrated. Some doctors recommend offering Pedialyte or another brand of rehydrating electrolyte solution in addition to formula or breast milk. Electrolyte drinks help replace lost fluids and minerals such as potassium, sodium, and magnesium. Try different brands and flavors until you find one your baby likes. If your child won’t swallow the electrolyte drink, just continue giving small amounts of formula or breast milk more frequently. If he refuses all liquids, contact your physician. If your baby is older, don’t be tempted to give him fruit juice as an alternative – it will only keep his stool loose. The illness typically lasts three to eight days, although the diarrhea may take longer to resolve.
“My baby seems short of breath.”
Unlike typical colds and flu, respiratory syncytial virus (RSV) can zero in on a baby’s lungs and lower respiratory tract, causing a fever, runny nose, hacking cough, and sometimes wheezing and shortness of breath.
RSV is a major cause of two serious lung conditions in babies under age 1, according to the CDC: bronchiolitis, an inflammation of the small airways; and viral pneumonia. As many as 40 percent of infants and young children have signs of one of these illnesses during their first RSV infection, such as wheezing, shortness of breath, or other difficulty breathing (all signs to see the doctor or go to the emergency room, stat).
Best Treatments for RSV: For most cases of mild RSV, treat your child as if he has a bad cold. Steroid medications have long been the mainstay treatment for bronchiolitis, but a recent study of 600 babies with moderate to severe bronchiolitis suggests that the medication is no more effective than a placebo, according to a report in The New England Journal of Medicine. Now doctors treat the condition with oxygen or IV fluids if needed, says Baltimore. Premature babies or those with lung or cardiac problems are most at risk for RSV complications, and they’re eligible for a medication that can help ward off infection. The shot is given monthly, from fall to spring, when RSV is most common. The virus can take as long as two weeks to run its course.
Deborah Pike Olsen is a freelance writer and mother of four in Weston, CT. This article originally appeared in Babytalk.
| Also see: Why Parents Should Say “Yes” to Immunizations for Their Children How to Keep Your Family Healthy When One Child Gets Sick |