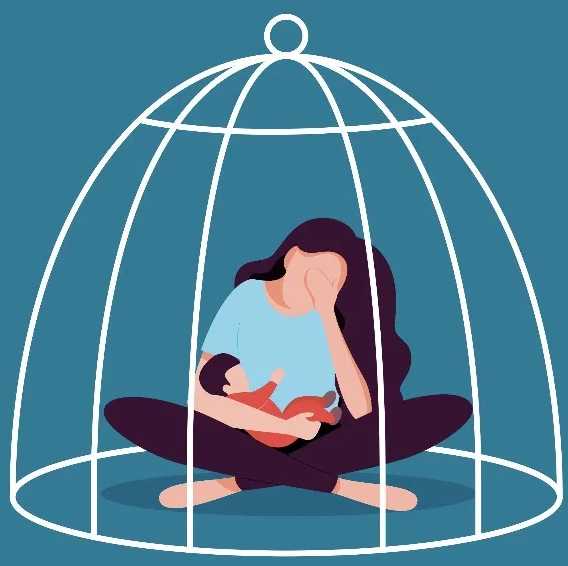
Is it Postpartum Depression or Baby Blues?
How to determine the difference between hormones and something more serious — and when to ask for help
Welcoming a new baby into your life comes with expected emotional ups and downs. Suddenly, you’re responsible for a tiny human who can’t even hold its head up yet – this kind of responsibility is overwhelming, to say the least. Toss in the dramatic hormone fluctuations that come naturally after giving birth, plus the physical toll of recovery, and it’s a wonder how a new parent wouldn’t feel a little out of control.
Still, as normal as it is to feel a mix of highs and lows in the first few weeks after having a baby, often known as the “baby blues,” it’s essential to stay alert and monitor what you’re feeling, as you may be experiencing postpartum depression (PPD).
Psst… Check Out NYC Faces Rising Challenges in Postpartum Care
To help make the distinction between the baby blues and PPD, we spoke with Janel Coleman, LMSW, a doula and licensed psychotherapist at Madison Square Psychotherapy in Manhattan, and Jessica Vernon, MD, FACOG, PMH-C, an OB-GYN, author, and clinical director at Oula in Manhattan. Here’s what they had to say.
What’s the Difference Between Baby Blues and Postpartum Depression?
Around 85% of birthing parents experience symptoms of baby blues, while around 12.5% are diagnosed with PPD. Given how common the baby blues are, it’s no wonder why signs of depression are so easily overlooked. In fact, the symptoms of each are incredibly similar.
According to Coleman, symptoms of baby blues can include feelings of anxiety, sadness, tearfulness, difficulty concentrating, irritability, and difficulty sleeping (even when baby is sleeping). These are all also signs of PPD, but according to Dr. Vernon, the difference is in the onset, duration, and severity of these symptoms.
Baby Blues
“Baby blues are a common and temporary emotional experience during the postpartum period … they typically occur within the first two weeks after the baby is born,” explains Coleman. Dr. Vernon describes the symptoms more as mood swings. “You may be laughing one minute and crying the next, often not even knowing why you are crying, then just as quickly changing again to a happier state,” she says. Dr. Vernon explains that these dramatic mood changes can be attributed to “rapid hormonal shifts that occur after the baby is born” and typically level out within the first two weeks after delivery.
In addition to being short-lived, baby blue symptoms are less intense than PPD symptoms. Dr. Vernon says, “The lows are not severe or persistent – you can easily ‘snap out of it.’” Also, while they can certainly feel overwhelming in the moment, Coleman notes that baby blues symptoms typically aren’t severe enough to interfere with a new parent’s ability to care for their baby or themselves.
Postpartum Depression
Just like the baby blues, symptoms of PPD can show up within the first two weeks of the postpartum period, but they won’t fizzle out. Both Dr. Vernon and Coleman stress that symptoms lasting longer than those first two weeks after baby arrives indicate it’s more than baby blues.
Not only do the symptoms last longer, but they’re also more intense with PPD. Coleman explains that these symptoms can become so severe that they can interfere with a parent’s ability to meet the needs of their baby. In some cases, the parent is able to care for the baby, but they stop taking care of themselves — they may stop eating or drinking, skip basic hygiene tasks for days on end, withdraw from family and friends, or not get enough sleep (beyond the typical parents-of-newborn sleep deprivation).
Symptoms that PPD shares with the baby blues but will be more severe include:
- Anxiety
- Irritability
- Feelings of sadness
- Difficulty concentrating
- Tearfulness
- Difficulty sleeping
Additional symptoms Coleman says to look for include:
- Feelings of hopelessness
- Difficulty bonding with baby
- Lack of interest in pleasurable activities
- Withdrawing from family and friends
- Doubts or fears about their ability to be a good parent
- Thoughts of harming themselves or baby
Postpartum Depression Treatment Options
In New York, the birthing parent’s health care provider screens them for postpartum depression (or postpartum mood disorders in general) during follow-up visits. However, these visits are usually not scheduled until several weeks after delivery. In 2023, the state passed legislation requiring pediatricians to perform maternal mental health screenings during baby well-visits, which occur within days of being released from the hospital.
Early identification, diagnosis, and treatment of PPD are essential for effective maternal mental health care. As part of the state’s effort to prioritize this, the Department of Health and the Office of Mental Health developed official guidance and standards for maternal depression screening and referrals, and insurers are required to cover screenings and treatment without prior authorization.
Once someone has been diagnosed with PPD, Dr. Vernon says their treatment plan will depend on how severe their symptoms are and what the patient wants. “[Treatment] is often a personal decision made with your care team,” she notes.
When a patient comes to her with PPD, Dr. Vernon says she checks to ensure they are not anemic, that their thyroid functions are normal, and that their vitamin D levels are optimized. “All of these things can contribute to symptoms of PPD,” she explains, and she will ensure the patient’s treatment plan also addresses these factors when appropriate.
Beyond these tests, Dr. Vernon says PPD treatment options can include a combination of psychotherapy, psychopharmacology (medication), peer support groups, and well-being practices (meditation, exercise, acupuncture, outdoor time, etc.).
Dr. Vernon also highlights the importance of sleep for those who are experiencing are and what the patient wants. “[Treatment] is often a personal decision made with your care team,” she notes.
When a patient comes to her with PPD, Dr. Vernon says she checks to ensure they are not anemic, that their thyroid functions are normal, and that their vitamin D levels are optimized. “All of these things can contribute to symptoms of PPD,” she explains, and she will ensure the patient’s treatment plan also addresses these factors when appropriate.
Beyond these tests, Dr. Vernon says PPD treatment options can include a combination of psychotherapy, psychopharmacology (medication), peer support groups, and well-being practices (meditation, exercise, acupuncture, outdoor time, etc.).
Dr. Vernon also highlights the importance of sleep for those who are experiencing postpartum depression. “One of the first recommendations mental health providers always give is to utilize your support system or bring in extra support so that you can get more sleep.” In cases where PPD interferes with the ability to sleep, a breastfeeding-safe sleep aid may be recommended.
Other Postpartum Mood Disorders
Postpartum depression is one of the more well-known postpartum mood disorders, but there are several others a new parent may also experience. Possible diagnoses include:
- Postpartum Anxiety
- Postpartum OCD
- Postpartum Panic Disorder
- Postpartum Bipolar Disorder
- Postpartum Post-Traumatic Stress Disorder
- Postpartum Psychosis
Coleman emphasizes that those who were diagnosed with mental health disorders prior to pregnancy or during pregnancy are 30% more likely to experience a postpartum mental health disorder.
It’s also worth noting that new parents can be diagnosed with more than one postpartum mood disorder at once. “You may experience one or many of these [mental health disorders], and seeing a provider trained in diagnosing them can be critical in understanding exactly what you are experiencing and what may best help you feel better,” says Dr. Vernon.
If you suspect you’re experiencing symptoms of postpartum depression or any other postpartum mood disorder, it’s essential to reach out to your provider for help. Your feelings are valid and shouldn’t be dismissed as “just hormones.” With the right treatment and care team, you can (and will) start feeling better.
Janel Coleman, LMSW, is a trained full-spectrum doula and a licensed psychotherapist at Madison Square Psychotherapy in New York City. Her focus areas include providing support during the trying-to-conceive, prenatal, and postpartum periods.
Jessica Vernon, MD, FACOG, PMH-C, is an OB-GYN and clinical director at Oula. She’s also an advocate for perinatal mental health, as well as the author of the book Then Comes Baby: An Honest Conversation About Birth, Postpartum, and the Complex Transition to Parenthood.
Psst… Check Out Postpartum Thyroiditis: The Hidden Hormonal Shift New Moms Should Know About